Michigan State University Secures $200,000 Grant to Develop Innovative Biomimetic Dressing for Chronic Wounds
The Institute for Quantitative Health Science & Engineering (IQ) at Michigan State University (MSU) has received a $200,000 research grant through MSU’s alliance with Corewell Health to pioneer a groundbreaking approach to treating chronic, hard-to-heal wounds. The project, led by MSU’s Dr. Nureddin Ashammakhi and Corewell Health’s Dr. Drue Orwig, focuses on creating an oxygen-generating, cell-based biomimetic dressing designed to revolutionize wound care, especially for patients with diabetes or poor blood flow.

Chronic wounds are particularly common among patients with diabetes or vascular diseases, and they are notoriously challenging to treat. Poor blood supply and reduced cell function slow the delivery of oxygen and nutrients to damaged tissue, which can lead to severe infections, prolonged suffering, and even limb amputation. Current treatments are limited in effectiveness, especially for underserved communities that lack access to specialized care.
The new biomimetic dressing will address these challenges by delivering oxygen and healing cells directly to the wound site. “Our goal is to create a multifunctional dressing that addresses the biological challenges of chronic wounds,” Dr. Ashammakhi explains. “By directly delivering oxygen, cells and healing-supporting biomaterials, we hope to improve wound healing outcomes significantly.”
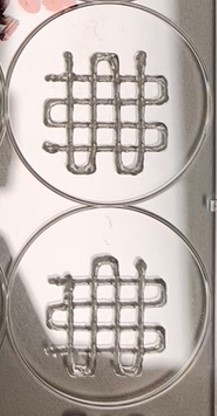
The team is designing a unique bandage using three-dimensional (3D) printing and electrospinning techniques. A biomimetic approach means that the dressing is designed to mimic the body’s natural structures and functions, replicating aspects of healthy tissue. By imitating these natural properties, biomimetic materials can better integrate with the body, support cell function, and promote faster healing.
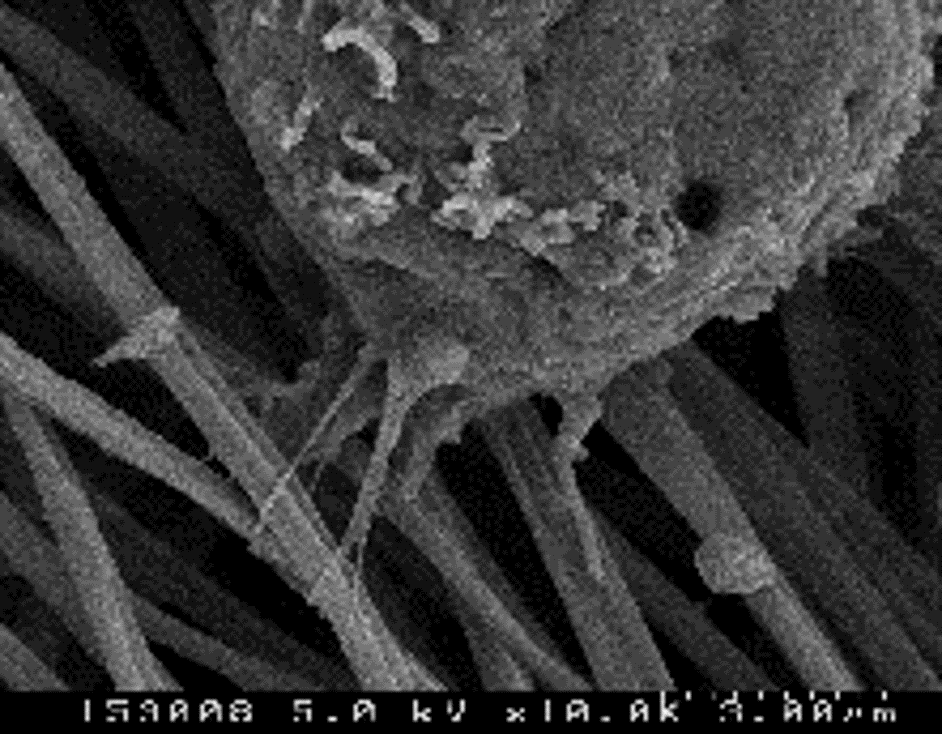
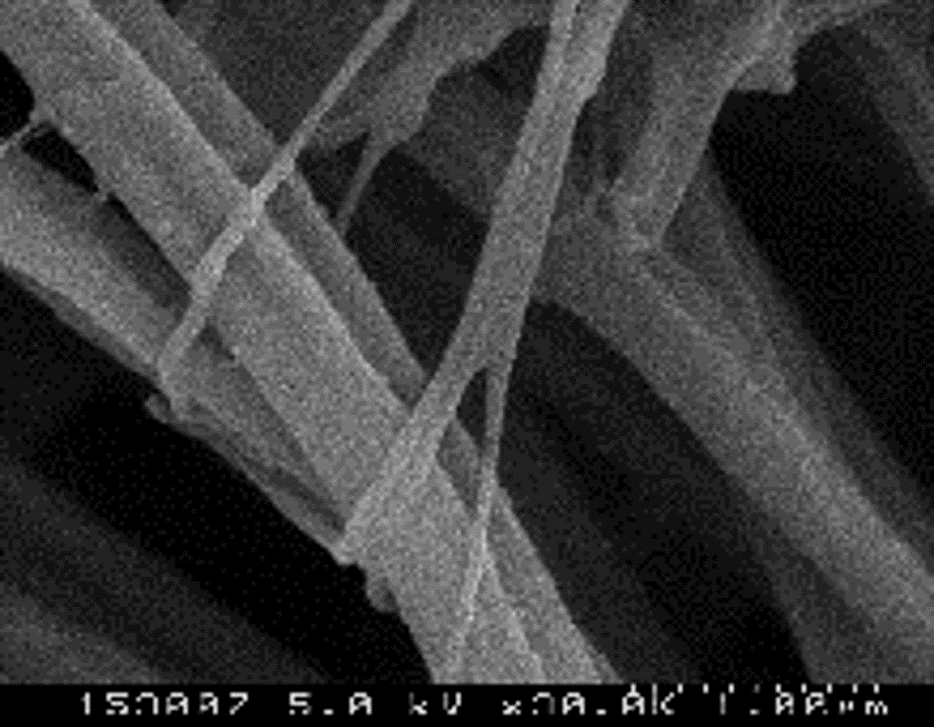
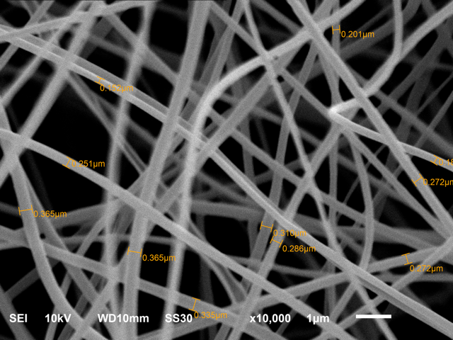
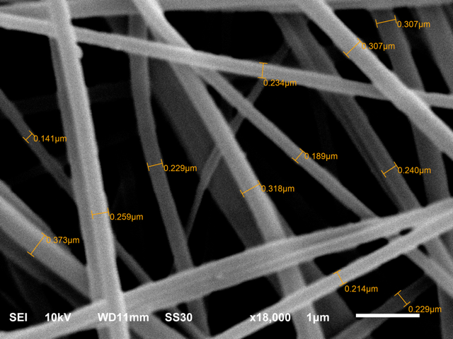
Electrospinning is a technique used to create extremely thin, fiber-like structures from synthetic or natural materials. In this process, an electric field pulls a liquid solution into fine fibers, forming a mat that closely resembles natural tissue scaffolding. This nanofiber mat can be customized to release oxygen steadily at the wound site, which improves cell function and provides an environment conducive to healing and infection control.
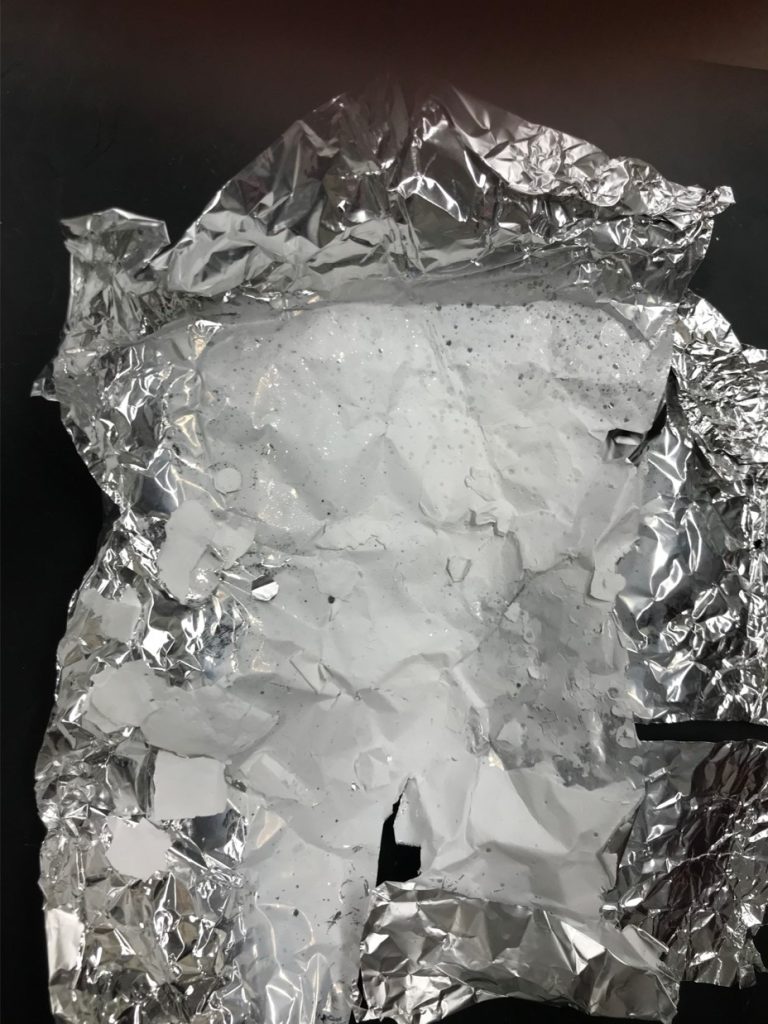
Using advanced 3D bioprinting, mesenchymal stem cells (MSCs), which are known for their regenerative properties, will be embedded in 3D-bioprinted scaffolds. MSCs can differentiate into various cell types, making them particularly effective in tissue regeneration. These constructs are also designed to release oxygen to maintain cell vitality, even in low-oxygen environments.

By combining oxygen-releasing nanofibers with MSC-laden constructs, these dressings deliver oxygen and healing cells simultaneously. This multifunctional approach addresses both the infection risk and the cellular damage typical of chronic wounds, adapting to wounds of varying severity.
The anticipated benefits extend beyond simple wound coverage. These dressings aim to address key barriers in chronic wound care, such as infection control and prolonged healing times. The project will test the materials in laboratory and controlled animal models, comparing their efficacy to traditional wound treatment.
This project brings together experts from MSU’s IQ and Corewell Health, with material science insights from Dr. Xanthippi Chatzistavrou of Thessaloniki University. Dr. Ashammakhi’s lab will focus on biomaterial synthesis and 3D bioprinting, while Dr. Scott Calabrese-Barton’s lab will develop the electrospun fiber components. IQ’s Dr. Christopher Contag’s cell biology lab will also be involved, and Corewell Health’s Austin Goodyke and Dr. Orwig will oversee clinical testing preparations and provide feedback on prototype refinement. The collaboration ensures that each institution’s specialized knowledge contributes to the project’s success.
In the short term, this project aims to produce a multifunctional live dressing for chronic wounds that provides faster, more reliable healing. Longer-term, the project could expand access to advanced wound care, particularly for patients with co-morbidities that worsen wound complications. By reducing the need for high-cost treatments like hyperbaric oxygen therapy, which are regionally limited and often inaccessible for underserved populations, the oxygen-generating bandage could make effective chronic wound treatment available in home-based settings, thus increasing health equity.
Over the next 18 months, the team will develop and test a series of prototypes for wounds of varying severity:
- Oxygen-Releasing Nanofiber Sheet: A standalone solution for minor wounds.
- 3D Bioprinted Construct with Stem Cells: Targeted for deeper wounds requiring cellular regeneration.
- Composite Constructs: A combination of the nanofiber sheet and bioprinted construct for complex wounds needing both oxygen and cell support.
By the project’s end, the team expects to have several ready-to-test prototypes, marking a significant advancement in wound-dressing capabilities. This partnership not only enhances healing rates but also aligns with MSU’s goal of health equity by developing accessible, affordable treatment options.
For updates on Dr. Ashammakhi’s work and IQ’s commitment to pioneering health science, stay connected with IQ at Michigan State University.

