Published in MSU Today February 16, 2024
Thanks to advancements in the development of patented synthetic human-like hearts first created at Michigan State, researchers can study human heart development and congenital heart disease on highly accurate models. This is facilitating the development of new therapies and pharmaceutical drugs to treat a variety of heart-related diseases just in time for the observance of American Heart Month in February.
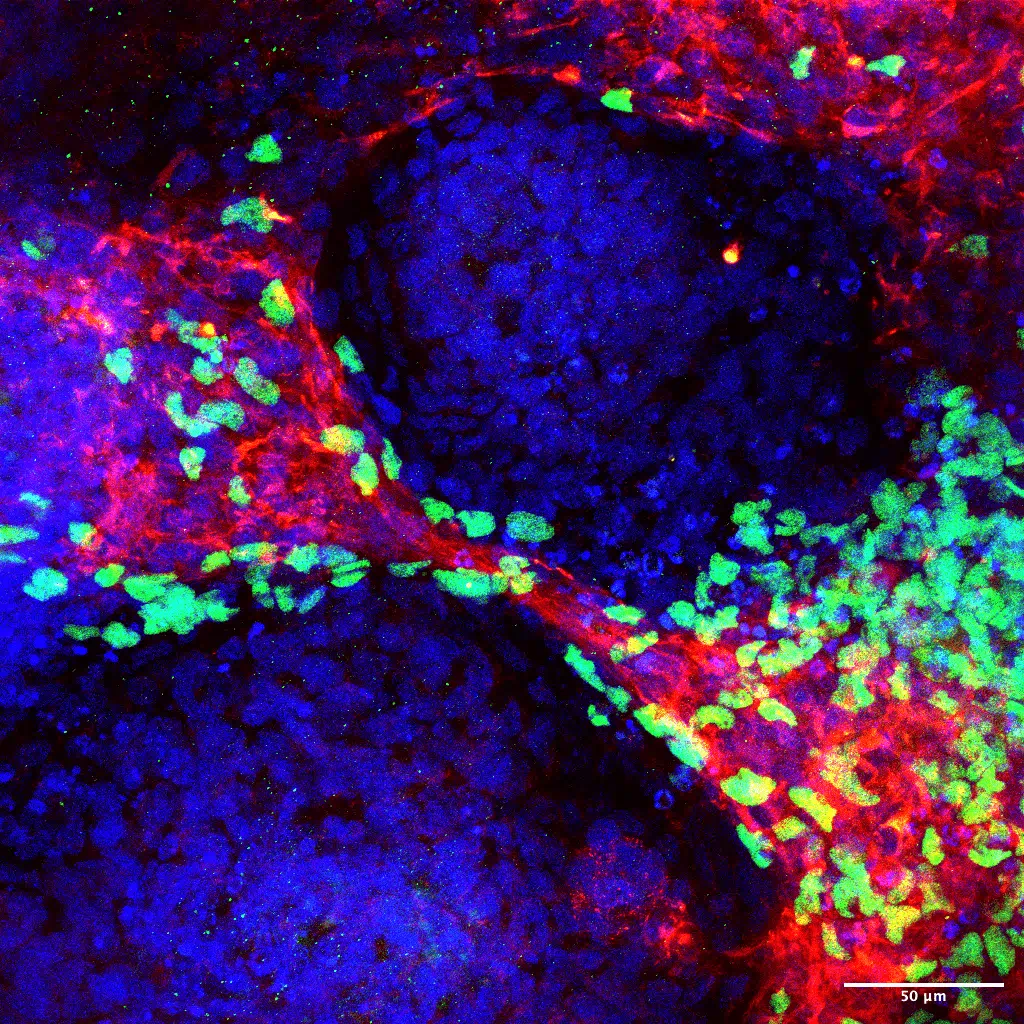
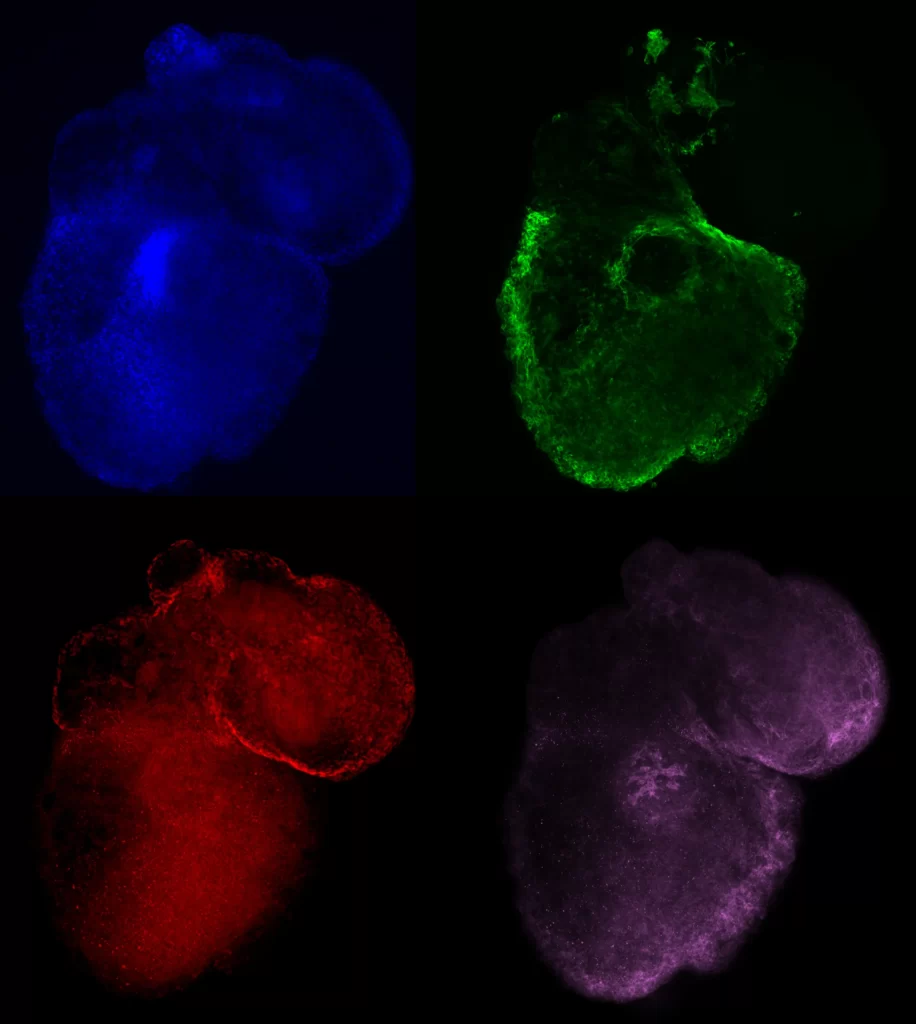
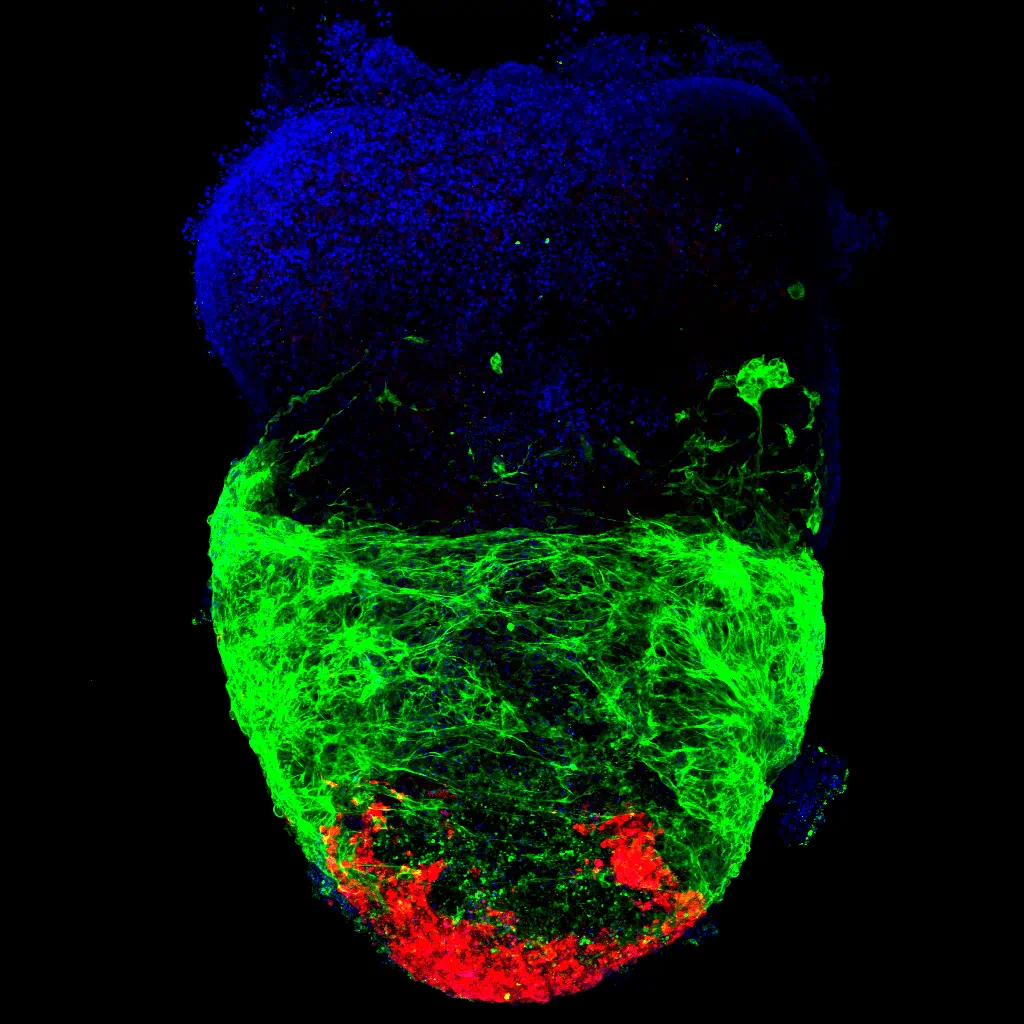
Similar in size and development to fetal human hearts, these mini heart organoids are becoming increasingly complex and realistic. The MSU research team that created the mini hearts first published their findings in 2020. They have quickly become a world leader in this field and their latest advancements have been published in Nature Communications and Stem Cell Reports. Another article appeared in November on the website for the National Institute of Health National Heart, Lung and Blood Institute.
Aitor Aguirre, associate professor of biomedical engineering and chief of the division of developmental and stem cell biology in MSU’s Institute for Quantitative Health Science and Engineering, explained that the introduction of realistic models is essential to the discovery of effective and clinically translatable solutions to cardiovascular disease. An estimated 21 million annual deaths are related to this condition, including disorders of the heart and blood vessels. And that number is growing.
“Although 90 percent of cardiovascular disease is thought to be preventable, it has become the leading cause of death in the developed world,” Aguirre said. “Thanks to advancements in stem cell technologies and bioengineering, we can grow and study human hearts. This will revolutionize medical approaches to treating and preventing heart diseases and congenital conditions by helping us understand the mechanisms of disease.
“In the future, we expect that fewer patients will need treatment and for those who do, the development of new drugs will take less time,” he added. “For congenital defects in particular, prevention is the best solution. This is why the mini heart organoids can really change the way we approach health care.”
As an example, Aguirre explained that pharmaceutical companies will pull drugs from the market if they are found to cause cardiotoxicity. To be able to predict toxicity in advance could save money, time and reduce the risk of drug failure.
The mini heart organoids are developed with donated pluripotent stem cells from adults. Their cellular complexity and physiological relevance enable the study of human heart development and disease in a dish to a degree previously unseen.
“We created a model using these organoids to study the effects of maternal diabetes at every stage of development in the fetal heart,” Aguirre said. “This is the definition of precision medicine. We can use science to make clinical practice more precise.”